Principles for putting evidence-based guidance into practice

Evidence and experience shows that using evidence-based guidance and improving practice is easier and more likely to happen when the environment for change is right. The following principles create and nurture a positive environment for change and help everyone deliver high-quality care and services.
Commitment to quality improvement
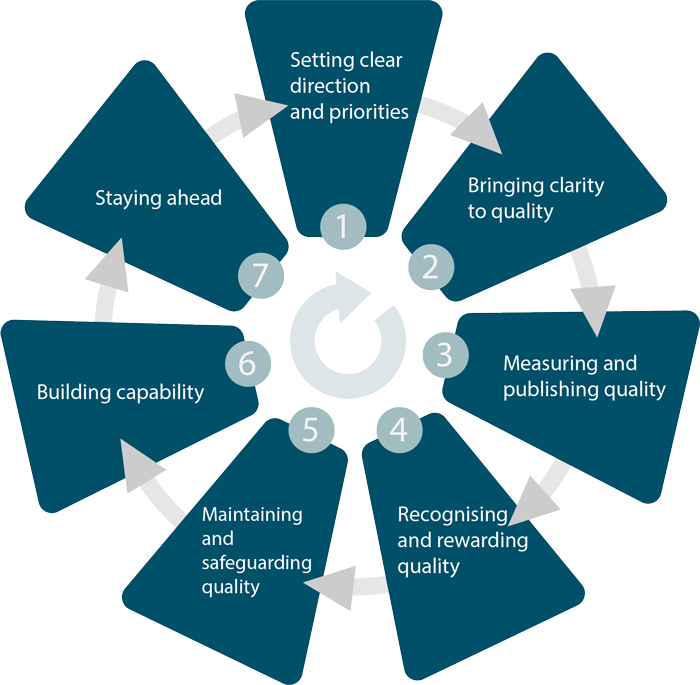
In 'A shared commitment to quality', national organisations responsible for overseeing quality across the NHS, public health and social care have agreed 7 steps to improve quality. These steps set out what all of us need to do to maintain and improve the quality of care that people experience. Quality matters also supports these 7 steps and aims to deliver high-quality, person-centred, adult social care.
| 1 | Setting clear direction and priorities based on evidence. See Practical steps for more on how to do this. |
| 2 | Bringing clarity to quality, NICE quality standards specify what high-quality care looks like. |
| 3 | Measuring and publishing quality, there are some ideas on how to do this in Practical steps. |
| 4 | Recognising and rewarding quality by celebrating and sharing good and outstanding care. There are some ideas on how to do this in Practical steps. |
| 5 | Maintaining and safeguarding quality, NICE quality standards can be used to measure quality. |
| 6 | Building capability, by improving leadership, management, professional and institutional culture, skills and behaviours to assure quality and sustain improvement. |
| 7 | Staying ahead, by developing research, innovation and planning to provide progressive, high-quality care. |
National programmes working to improve quality use our guidance and standards to underpin their work. For example, Getting it Right First Time and NHS RightCare aim to improve care by reducing variation.
A commitment to quality improvement methods and continuous learning is a feature of many health and social care organisations rated ‘outstanding’ by the Care Quality Commission (CQC). Using NICE guidance can help you monitor progress or show compliance with national standards and using NICE quality standards can help you demonstrate outstanding performance.
Liz Mouland, Chief Nurse at First Community Health and Care said: "The culture of an organisation is crucial in ensuring that staff can innovate and test new approaches to care in order to deliver high quality and cost-efficient services. As an organisation rated outstanding by CQC, the board are committed to, and encourage professional curiosity within a robust governance framework to supporting staff to embed a continuous quality improvement cycle".
The 7 steps to quality improvement
The 7 steps to quality improvement
Effective leadership
Successful change processes have strong, effective leadership. And not just at the top; visible, proactive and inspiring leadership is seen at all levels (individual, team, organisational and national).
Effective leaders are committed to providing safe, effective and efficient, high-quality care and services. They build trust across organisational and professional boundaries and with people using services. They are compassionate, inclusive and focused on continuous improvement. This motivates staff at every level to have high aspirations for themselves and others. Consistent reporting on service outcomes, celebrating success and learning from failure, all help to create an organisation that is open to change and ready to learn.
Leaders need to create change agency: the power individually and collectively to make a positive difference. This empowers everyone to push the boundaries of what is possible and make change happen more quickly; transforming care and services.
Liz Mouland, Chief Nurse at First Community Health and Care said "Every member of our board is committed to promoting evidence-based practice. These principles, values and behaviours are role-modelled across First Community Health and Care and all quality improvements are shared and celebrated across the organisation."
The right culture
Traditionally ‘power’ is held by the leaders. It works like a currency and is transaction based. It is about governance, hierarchy and systems. It is difficult to imagine how we would work without it. However, power is shifting. New power works differently, it is like a current: it flows and connects people. It is made by many, it’s open and collaborative.
An organisation’s culture shapes the behaviour of everyone in the organisation and directly affects the quality of care they provide. We know that staff who gain pride and joy from their work and shared values perform better. By finding a way to balance ‘new power’ and ‘old power’organisations can foster a positive, open culture focused on quality improvement.
Emma Marcroft, Head of Patient Safety and Quality, First Community Health and Care said: "Becoming a community interest company was an opportunity for us to rethink. We took the opportunity to embed an open culture focused on improving and learning. We made sure NICE was prioritised at the start and continue to develop and refine this, supporting each other to identify gaps, implement recommendations and measure impact".
Helen Hanks, Quality Improvement Manager, Devon Partnership Trust said: "Reviewing and changing the way meetings were organised led to increased engagement and a change of culture. The meetings are chaired by the trust’s medical director and attended by leads from each directorate along with other key personnel from different disciplines. We are creating a culture of positive challenge, accountability and transparency."
If you want to find out more, see Jeremy Heimans and Henry Timms article on Understanding new power. For more on shared values see the NHS constitution.
Working together
The most successful improvement projects are the result of working with people with different perspectives and skills who work in the service or are affected by the service. By co-producing a new or improved service, you build on everyone’s experiences and make sure that any changes genuinely support people using the service as well as staff. Ensuring opportunities to keep the conversation going means you can shape the service as it develops.
Our guidance and standards can help to provide a common framework for co-production.
Joanna Smith, manager, Healthwatch Isle of Wight said: "We wanted to ensure everyone was involved in improving the service. We spoke to residents and relatives and people working in the local authority, primary care, and care home managers."
Emma Marcroft, Head of Patient Safety and Quality, First Community Health and Care said: "Our biggest challenge, in developing our organisation’s focus on NICE was ensuring ownership by all of our staff. It is important to consult with our staff at every stage to find out what works and what doesn’t. Initially, we were met by a lack of understanding and buy-in. A positive and open culture which facilitates staff engagement and innovation has ensured that we now have a robust process in place."
If you want to find out more, the Social Care Institute for Excellence’s guide on co-production is focused on social care but could be used in other sectors.